








Biotechnology Bulletin ›› 2022, Vol. 38 ›› Issue (3): 181-187.doi: 10.13560/j.cnki.biotech.bull.1985.2021-0630
Previous Articles Next Articles
ZHONG Ming-yue1( ), LIU Chun-yan1, YAN Yan1, ZHANG Xiao-hui1, YUAN Hai-sheng1, XU Guo-quan1, ZHANG He-ping2, WANG Yu-zhen1(
), LIU Chun-yan1, YAN Yan1, ZHANG Xiao-hui1, YUAN Hai-sheng1, XU Guo-quan1, ZHANG He-ping2, WANG Yu-zhen1( )
)
Received:2021-05-17
Online:2022-03-26
Published:2022-04-06
Contact:
WANG Yu-zhen
E-mail:627401932@qq.com;wangyuzhen817@126.com
ZHONG Ming-yue, LIU Chun-yan, YAN Yan, ZHANG Xiao-hui, YUAN Hai-sheng, XU Guo-quan, ZHANG He-ping, WANG Yu-zhen. Improvement Effect of Bifidobacterium lactis V9 on NAFLD Rats Induced by High-fat Diet[J]. Biotechnology Bulletin, 2022, 38(3): 181-187.
| 脂肪 Fat/% | 蛋白质 Protein/% | 碳水化合物 Carbohydrate/% | |
|---|---|---|---|
| 普通维持饲料 Ordinaryl feed | 11.4 | 27.5 | 65.8 |
| 高脂饲料High-fat diet (HFD) | 33.1 | 19.6 | 47.1 |
Table 1 Ratio of animal feed
| 脂肪 Fat/% | 蛋白质 Protein/% | 碳水化合物 Carbohydrate/% | |
|---|---|---|---|
| 普通维持饲料 Ordinaryl feed | 11.4 | 27.5 | 65.8 |
| 高脂饲料High-fat diet (HFD) | 33.1 | 19.6 | 47.1 |
| 引物名称 Primer name | 引物序列 Primer sequence |
|---|---|
| IL-1β antisense | 5'-GAATGCCACCTTTTGACAGTG-3' |
| IL-1β sense | 5'-TGGATGCTCTCATCAGGACAG-3' |
| TNF-α antisense | 5'-TTGATGGTGGTGCATGAGAG-3' |
| TNF-α sense | 5'-AAACACAAGATGCTGGGACA-3' |
| TLR2 antisense | 5'-CTCCTGTGAACTCCTGTCCTT-3' |
| TLR2 sense | 5'AGCTGTCTGGCCAGTCAAC-3' |
| TLR9 antisense | 5'-CCGAAGACCTAGCCAACCT-3' |
| TLR9 sense | 5'-TGATCACAGCGACGGCAATT-3' |
| Fas antisense | 5'-GAGCGTTCGTGAAACCGACA-3' |
| Fas sense | 5'-AGGTTGGTGCACCTCCACTTG-3' |
| Fabp1 antisense | 5'-TTCCCCAGTCATGGTCTCCA-3' |
| Fabp1 sense | 5'-TCATGAAGGCGATGGGTCTG-3' |
| ZO-1 antisense | 5'-CCATCTTTGGACCGATTGCTG-3' |
| ZO-1 sense | 5'-TAATGCCCGAGCTCCGATG-3' |
| Occludin antisense | 5'-TTGGGAGCCTTGACATCTTGTTC-3' |
| Occludin sense | 5'-GCCATACATGTCATTGCTTGGTG-3' |
| GAPDH antisense | 5'-AGGTCGGTGTGTGAACGGATTTG-3' |
| GAPDH sense | 5'-TGTAGACCATGTAGTTGAGGTCA-3' |
Table 2 Primer sequences of real-time PCR
| 引物名称 Primer name | 引物序列 Primer sequence |
|---|---|
| IL-1β antisense | 5'-GAATGCCACCTTTTGACAGTG-3' |
| IL-1β sense | 5'-TGGATGCTCTCATCAGGACAG-3' |
| TNF-α antisense | 5'-TTGATGGTGGTGCATGAGAG-3' |
| TNF-α sense | 5'-AAACACAAGATGCTGGGACA-3' |
| TLR2 antisense | 5'-CTCCTGTGAACTCCTGTCCTT-3' |
| TLR2 sense | 5'AGCTGTCTGGCCAGTCAAC-3' |
| TLR9 antisense | 5'-CCGAAGACCTAGCCAACCT-3' |
| TLR9 sense | 5'-TGATCACAGCGACGGCAATT-3' |
| Fas antisense | 5'-GAGCGTTCGTGAAACCGACA-3' |
| Fas sense | 5'-AGGTTGGTGCACCTCCACTTG-3' |
| Fabp1 antisense | 5'-TTCCCCAGTCATGGTCTCCA-3' |
| Fabp1 sense | 5'-TCATGAAGGCGATGGGTCTG-3' |
| ZO-1 antisense | 5'-CCATCTTTGGACCGATTGCTG-3' |
| ZO-1 sense | 5'-TAATGCCCGAGCTCCGATG-3' |
| Occludin antisense | 5'-TTGGGAGCCTTGACATCTTGTTC-3' |
| Occludin sense | 5'-GCCATACATGTCATTGCTTGGTG-3' |
| GAPDH antisense | 5'-AGGTCGGTGTGTGAACGGATTTG-3' |
| GAPDH sense | 5'-TGTAGACCATGTAGTTGAGGTCA-3' |
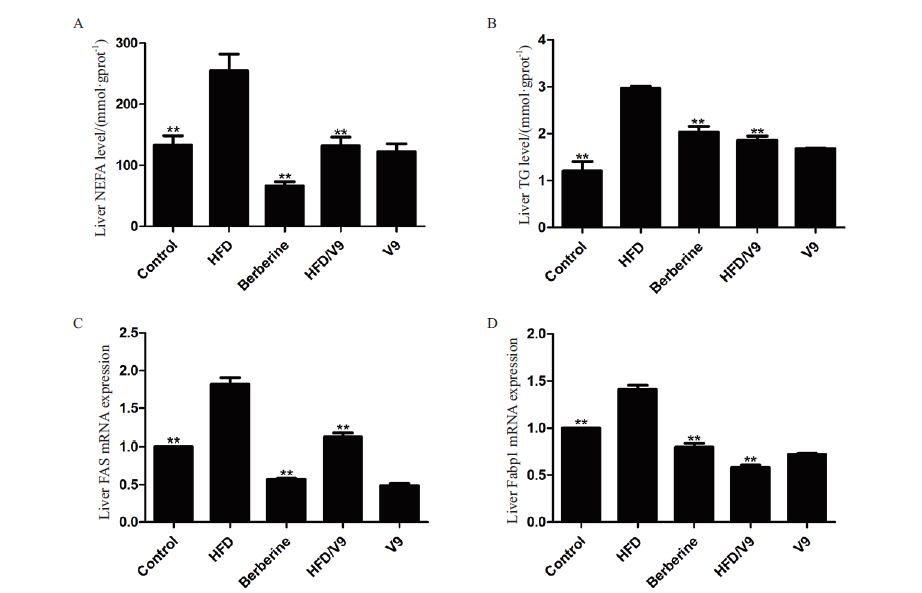
Fig. 1 Contents of NEFA and TG,and mRNA expression of FAS and Fabp1 in the liver ** Refers to the comparison between the Control group,Berberin group,and HFD/V9 group with the HFD group,P<0.01,the same bleow
| [1] |
Liu JY, Ayada I, Zhang XF, et al. Estimating global prevalence of metabolic dysfunction-associated fatty liver disease in overweight or obese adults[J]. Clin Gastroenterol Hepatol, 2021. DOI: 10.1016/j.cgh,2021.02.030.
doi: 10.1016/j.cgh,2021.02.030 |
| [2] |
Diehl AM, Day C. Cause, pathogenesis, and treatment of nonalcoholic steatohepatitis[J]. N Engl J Med, 2017, 377(21):2063-2072.
doi: 10.1056/NEJMra1503519 URL |
| [3] | M I, Singh C, Ganie MA, et al. NASH:The hepatic injury of metabolic syndrome:a brief update[J]. Int J Health Sci:Qassim, 2009, 3(2):265-270. |
| [4] | İlyas TUNCER, Hanefi ÖZBEK, Topal C, et al. The serum levels of IL-1b, IL-6, IL-8 and TNF-a in nonalcoholic fatty liver[J]. Turkish Journal of Medical Sciences, 2003, 33(24):381-386. |
| [5] |
Day CP, James OF. Steatohepatitis:a tale of two “hits” ?[J]. Gastroenterology, 1998, 114(4):842-845.
pmid: 9547102 |
| [6] |
Buzzetti E, Pinzani M, Tsochatzis EA. The multiple-hit pathogenesis of non-alcoholic fatty liver disease(NAFLD)[J]. Metabolism, 2016, 65(8):1038-1048.
doi: 10.1016/j.metabol.2015.12.012 URL |
| [7] |
Fang YL, Chen H, Wang CL, et al. Pathogenesis of non-alcoholic fatty liver disease in children and adolescence:From “two hit theory” to “multiple hit model”[J]. World J Gastroenterol, 2018, 24(27):2974-2983.
doi: 10.3748/wjg.v24.i27.2974 URL |
| [8] |
Tilg H, Moschen AR. Evolution of inflammation in nonalcoholic fatty liver disease:The multiple parallel hits hypojournal[J]. Hepatology, 2010, 52(5):1836-1846.
doi: 10.1002/hep.v52:5 URL |
| [9] |
Rinaldi L, Pafundi PC, Galiero R, et al. Mechanisms of non-alcoholic fatty liver disease in the metabolic syndrome. A narrative review[J]. Antioxidants, 2021, 10(2):270.
doi: 10.3390/antiox10020270 URL |
| [10] |
Li ZP, Yang SQ, Lin HZ, et al. Probiotics and antibodies to TNF inhibit inflammatory activity and improve nonalcoholic fatty liver disease[J]. Hepatology, 2003, 37(2):343-350.
doi: 10.1053/jhep.2003.50048 URL |
| [11] |
Sun ZH, Chen X, Wang JC, et al. Complete genome sequence of probiotic Bifidobacterium animalis subsp. lactis strain V9[J]. J Bacteriol, 2010, 192(15):4080-4081.
doi: 10.1128/JB.00369-10 URL |
| [12] | 陈霞. 具有益生功能的Bifidobacterium animalis subsp. lactis V9的安全性评估、生理功效及其全基因组学研究[D]. 呼和浩特:内蒙古农业大学, 2010. |
| Chen X. Safety evaluation, physiological function & whole genome sequence of potential probiotic Bifidobacterium animalis subsp. lactis V9[D]. Hohhot:Inner Mongolia Agricultural University, 2010. | |
| [13] |
Wong WK, Chan WK. Nonalcoholic fatty liver disease:a global perspective[J]. Clin Ther, 2021, 43(3):473-499.
doi: 10.1016/j.clinthera.2021.01.007 URL |
| [14] | Dongiovanni P, Paolini E, Corsini A, et al. NAFLD or MAFLD diagnoses and cardiovascular diseases:from epidemiology to drug approaches[J]. European Journal of Clinical Investigation, 2021, 14(5):e13519. |
| [15] |
Cai GS, Su H, Zhang J. Protective effect of probiotics in patients with non-alcoholic fatty liver disease[J]. Medicine, 2020, 99(32):e21464.
doi: 10.1097/MD.0000000000021464 URL |
| [16] |
Kwong EK, Puri P. Gut microbiome changes in nonalcoholic fatty liver disease & alcoholic liver disease[J]. Transl Gastroenterol Hepatol, 2021, 6:3.
doi: 10.21037/tgh.2020.02.18 pmid: 33409398 |
| [17] |
Bajaj JS, Heuman DM, Hylemon PB, et al. Randomised clinical trial:Lactobacillus GG modulates gut microbiome, metabolome and endotoxemia in patients with cirrhosis[J]. Aliment Pharmacol Ther, 2014, 39(10):1113-1125.
doi: 10.1111/apt.2014.39.issue-10 URL |
| [18] |
Yan Y, Liu C, Zhao S, et al. Probiotic Bifidobacterium lactis V9 attenuates hepatic steatosis and inflammation in rats with non-alcoholic fatty liver disease[J]. AMB Express, 2020, 10(1):101.
doi: 10.1186/s13568-020-01038-y pmid: 32472368 |
| [19] |
Kumar R, Goh BG, Kam JW, et al. Comparisons between non-alcoholic steatohepatitis and alcohol-related hepatocellular carcinoma[J]. Clin Mol Hepatol, 2020, 26(2):196-208.
doi: 10.3350/cmh.2019.0012 URL |
| [20] |
Zhou HP, Urso CJ, Jadeja V. Saturated fatty acids in obesity-associated inflammation[J]. J Inflamm Res, 2020, 13:1-14.
doi: 10.2147/JIR URL |
| [21] | 蒋李妍, 肖新华. 肠道菌群与非酒精性脂肪肝病相关性研究进展[J]. 临床与病理杂志, 2016, 36(12):2060-2065. |
| Jiang LY, Xiao XH. Research progress on correlation between gut microbiota and non-alcoholic fatty liver disease[J]. J Clin Pathol Res, 2016, 36(12):2060-2065. | |
| [22] | Dai X, Wang BM. Role of gut barrier function in the pathogenesis of nonalcoholic fatty liver disease[J]. Gastroenterol Res Pract, 2015, 2015:1-6. |
| [1] | XIE Guo-zhen, TANG Yuan, NING Xiao-mei, QIU Ji-hui, TAN Zhou-jin. Effects of Dendrobium officinale Polysaccharides on the Intestinal Mucosal Structure and Microbiota in Mice Fed a High-fat Diet [J]. Biotechnology Bulletin, 2022, 38(2): 150-157. |
| [2] | YANG Li-jie, ZENG Xiang-fang, QIAO Shi-yan. Research Advances on Non-starch Polysaccharide in the Regulation of Intestinal Microflora in Pigs [J]. Biotechnology Bulletin, 2020, 36(2): 9-16. |
| [3] | MA Tao, DIAO Qi-yu. Recent Advance in the Study of the Regulation of Early Life Gut Microbiota by Probiotics in Livestock [J]. Biotechnology Bulletin, 2020, 36(2): 17-26. |
| [4] | YU Jie, LIU Xin, ZHANG Chi, ZHAO Ji-chun, LI Fu-hua, MING Jian. Anti-aging Effect and Molecular Mechanism of Probiotics:A Review [J]. Biotechnology Bulletin, 2020, 36(1): 167-174. |
| [5] | DU Ruo-xi, GUO Ming-zhang, XIE Zi-xin, HE Xiao-yun, HUANG Kun-lun, XU Wen-tao. Application and Prospect of Synthetic Biology in Improving Intestinal Health [J]. Biotechnology Bulletin, 2018, 34(1): 49-59. |
| [6] | WANG Li-jie, YU Xiao-bin, FANG Yin-bing, GU Qiu-ya. Screening of Probiotics for Inhibiting Pathogens and Preliminary Determination of Antimicrobial Substances [J]. Biotechnology Bulletin, 2017, 33(11): 123-129. |
| [7] | Xin Yueqiang, Liang Rongrong, Wang Ruiming. Effects of Galactooligosaccharide on Exopolysaccharide Produced by Intestinal Probiotics [J]. Biotechnology Bulletin, 2015, 31(6): 144-150. |
| [8] | Sun Hongmei, Wang Tengfei, Li Piwu, Tang Weihua, Qu Lina, Wang Ruiming . Tolerance of Three Potentially Piglets Feed Probiotic and Antagonistic Pathogens Research [J]. Biotechnology Bulletin, 2013, 0(8): 155-159. |
| [9] | Xu Defeng, Li Caihong, Sun Lijun, Wang Yaling, Ye Riying. Comparative Analysis of Extraction Method in Genome DNA from Intestinal Microflora of Penaeus vannamei [J]. Biotechnology Bulletin, 2013, 0(12): 119-122. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||