







生物技术通报 ›› 2022, Vol. 38 ›› Issue (9): 59-71.doi: 10.13560/j.cnki.biotech.bull.1985.2022-0854
• 细菌耐药性专题(专题主编: 刘雅红 教授 孙坚 教授) • 上一篇 下一篇
赵艳坤1( ), 刘慧敏2, 孟璐2, 王成1, 王加启2, 郑楠2(
), 刘慧敏2, 孟璐2, 王成1, 王加启2, 郑楠2( )
)
收稿日期:2022-07-10
出版日期:2022-09-26
发布日期:2022-10-11
作者简介:赵艳坤,女,博士,副研究员,研究方向:乳品营养与安全;E-mail: 基金资助:
ZHAO Yan-kun1( ), LIU Hui-min2, MENG Lu2, WANG Cheng1, WANG Jia-qi2, ZHENG Nan2(
), LIU Hui-min2, MENG Lu2, WANG Cheng1, WANG Jia-qi2, ZHENG Nan2( )
)
Received:2022-07-10
Published:2022-09-26
Online:2022-10-11
摘要:
大肠埃希菌(Escherichia coli)是人类和动物中常见细菌病原体,E.coli已对多种抗菌药物产生耐药,且由于抗菌药物选择压力越来越大,致使菌株的适应性和致病性更强,耐药的传播更快、定植率更高,给全球流行病学和临床治疗带来极大的挑战。近年来,E.coli的异质性耐药(heteroresistance,HR)相关研究相继被报道,异质性耐药是指细菌中的同源亚群对某种抗菌药物表现出不同的敏感性,是敏感菌进化为耐药菌的中间阶段,不同于完全耐药,异质性耐药在临床上不易及时检出,常导致临床抗菌药物治疗失败。因此,为有效防控E.coli感染及耐药的演变,深入剖析E.coli异质性耐药的流行特征及可能的机制尤为重要,本文就E.coli的异质性耐药研究进行了梳理,并对异质性耐药从表型特征、检测方法和可能的机制等方面进行了概述。旨在加强对E.coli异质性耐药的认识和研究,以期为全面了解E.coli耐药过程及发生机制、优化抗菌药物使用策略、减缓完全耐药菌种的出现提供参考。
赵艳坤, 刘慧敏, 孟璐, 王成, 王加启, 郑楠. 大肠埃希菌异质性耐药的研究进展[J]. 生物技术通报, 2022, 38(9): 59-71.
ZHAO Yan-kun, LIU Hui-min, MENG Lu, WANG Cheng, WANG Jia-qi, ZHENG Nan. Research Progress in Heteroresistance of Escherichia coli[J]. Biotechnology Bulletin, 2022, 38(9): 59-71.
| 方法 Methods | 优点 Advantages | 缺点 Disadvantages | 参考文献 Reference |
|---|---|---|---|
| E-test法、K-B纸片扩散法 E-test and Kirby-Bauer test | (1)传统、经典的药敏试验方法; (2)可用于异质性耐药的初筛; (3)操作简便、成本较低、结果直观易判读。 | (1)由于平板上的细胞密度低,不易检出低频率出现的耐药亚群; (2)可信度低,假阳性、假阴性检出率较高。 | [ |
| M-E-test法M-E-test method | (1)可用于异质性耐药的大规模筛选; (2)操作简单。 | 培养板上细胞密度越高,检测异质性耐药亚群的概率越高,但检测的准确率不稳定,易造成误判。 | [ |
| GRD E-test、琼脂筛选 GRD E-test and agar screen | (1)临床实验室常规使用的药敏试验方法; (2)用于观察某种程度的耐药性和异质性耐药性之间存在强烈相关性的简单筛选方法(hVISA)。 | (1)无法检测异质性耐药; (2)缺乏有关亚群频率和MIC的信息。 | [ |
| 微量肉汤稀释法 Broth microdilution(BMD) | 临床实验室常规使用的药敏试验方法。 | (1)在存在耐药亚群的情况下,MIC的读数高度依赖于耐药细菌的接种密度和生长速率; (2)没有关于耐药亚群频率的信息,其MIC信息较差; (3)操作繁琐。 | [ |
| 琼脂稀释 Agar dilution | 临床实验室常规使用的药敏试验方法。 | (1)使用耐药细菌的单个小菌落有可能错过低频率的亚群; (2)如果检测到异质性耐药,则提供有关耐药亚群的频率和MIC的少许信息; (3)耗时、费力。 | [ |
| 群体谱分析法 PAP test | (1)检测异质性耐药较可靠的方法;(2)能够提供有关耐药亚群频率和MIC的有效信息; (3)可定量分析、准确度高、稳定性好、可重复性好。 | (1)操作繁琐且成本昂贵; (2)耗时耗力; (3)技术性强,临床推广应用困难。 | [ |
| 微量稀释群体谱分析法 Microdilution PAP test | (1)比常规PAP测试更快、更便宜; (2)可得知耐药亚群的频率和MIC。 | 检测的效果取决于细胞密度,误差较大。 | [ |
| 改良群体谱分析曲线法 PAP-AUC | (1)hVISA检测的黄金标准; (2)准确性高。 | (1)步骤繁琐且成本昂贵; (2)参考hVISA菌株可能会对不同药物浓度具有高度依赖性的耐药亚群分离株进行错误分类,造成假阳性或假阴性结果。 | [ |
| 自动肉汤系统(如VITEK 2、MicroScan、WalkAway) Automated broth systems(for example,VITEK 2,MicroScan,and WalkAway) | 临床实验室常规使用药敏试验方法。 | 在检测耐药亚群方面效果不佳。 | [ |
| 分子检测方法(如探针分析和GeneXpert-Xpert-MTB/RIF-Ultra) Molecular detection methods(for example,line probe assays,GeneXpert Xpert MTB/RIF Ultra) | (1)与传统或自动检测方法相比,更能快速检测异质性耐药; (2)能够准确检测细菌亚群的点突变。 (3)有时可直接用于患者样本(如,结核分枝杆菌的痰样本)。 | (1)并非所有探针分析系统都能检测耐药亚群,检测效率和稳定性不稳定; (2)依赖于对耐药基因的全面了解,会造成结果差异较大,不适用于所有细菌。 | [ |
表1 异质性耐药的检测方法对比
Table 1 Comparison of detection methods for heteroresistance
| 方法 Methods | 优点 Advantages | 缺点 Disadvantages | 参考文献 Reference |
|---|---|---|---|
| E-test法、K-B纸片扩散法 E-test and Kirby-Bauer test | (1)传统、经典的药敏试验方法; (2)可用于异质性耐药的初筛; (3)操作简便、成本较低、结果直观易判读。 | (1)由于平板上的细胞密度低,不易检出低频率出现的耐药亚群; (2)可信度低,假阳性、假阴性检出率较高。 | [ |
| M-E-test法M-E-test method | (1)可用于异质性耐药的大规模筛选; (2)操作简单。 | 培养板上细胞密度越高,检测异质性耐药亚群的概率越高,但检测的准确率不稳定,易造成误判。 | [ |
| GRD E-test、琼脂筛选 GRD E-test and agar screen | (1)临床实验室常规使用的药敏试验方法; (2)用于观察某种程度的耐药性和异质性耐药性之间存在强烈相关性的简单筛选方法(hVISA)。 | (1)无法检测异质性耐药; (2)缺乏有关亚群频率和MIC的信息。 | [ |
| 微量肉汤稀释法 Broth microdilution(BMD) | 临床实验室常规使用的药敏试验方法。 | (1)在存在耐药亚群的情况下,MIC的读数高度依赖于耐药细菌的接种密度和生长速率; (2)没有关于耐药亚群频率的信息,其MIC信息较差; (3)操作繁琐。 | [ |
| 琼脂稀释 Agar dilution | 临床实验室常规使用的药敏试验方法。 | (1)使用耐药细菌的单个小菌落有可能错过低频率的亚群; (2)如果检测到异质性耐药,则提供有关耐药亚群的频率和MIC的少许信息; (3)耗时、费力。 | [ |
| 群体谱分析法 PAP test | (1)检测异质性耐药较可靠的方法;(2)能够提供有关耐药亚群频率和MIC的有效信息; (3)可定量分析、准确度高、稳定性好、可重复性好。 | (1)操作繁琐且成本昂贵; (2)耗时耗力; (3)技术性强,临床推广应用困难。 | [ |
| 微量稀释群体谱分析法 Microdilution PAP test | (1)比常规PAP测试更快、更便宜; (2)可得知耐药亚群的频率和MIC。 | 检测的效果取决于细胞密度,误差较大。 | [ |
| 改良群体谱分析曲线法 PAP-AUC | (1)hVISA检测的黄金标准; (2)准确性高。 | (1)步骤繁琐且成本昂贵; (2)参考hVISA菌株可能会对不同药物浓度具有高度依赖性的耐药亚群分离株进行错误分类,造成假阳性或假阴性结果。 | [ |
| 自动肉汤系统(如VITEK 2、MicroScan、WalkAway) Automated broth systems(for example,VITEK 2,MicroScan,and WalkAway) | 临床实验室常规使用药敏试验方法。 | 在检测耐药亚群方面效果不佳。 | [ |
| 分子检测方法(如探针分析和GeneXpert-Xpert-MTB/RIF-Ultra) Molecular detection methods(for example,line probe assays,GeneXpert Xpert MTB/RIF Ultra) | (1)与传统或自动检测方法相比,更能快速检测异质性耐药; (2)能够准确检测细菌亚群的点突变。 (3)有时可直接用于患者样本(如,结核分枝杆菌的痰样本)。 | (1)并非所有探针分析系统都能检测耐药亚群,检测效率和稳定性不稳定; (2)依赖于对耐药基因的全面了解,会造成结果差异较大,不适用于所有细菌。 | [ |
| 抗菌药物 名称 Antibiotic | 样品(来源) Sample (Sources) | 样本数 Number of samples | 异质性耐药测定方法Method for determination of heteroresistance | 异质性耐药率 Prevalence of heteroresistance/% | 耐药率Prevalence of resistance/% | 异质性耐药亚群的频次 Frequency of heteroresistant subpopulations | 国家/地区Country /Region | 文献 Reference |
|---|---|---|---|---|---|---|---|---|
| 亚胺培南 Imipenem | 医院分离株 | 11 | E-test(抑菌圈内菌落生长初步判定异质性) PAP(异质性耐药以MIC/NIC≥8来确定) | 0 | 0 | ND | 瑞典 | [ |
| 厄他培南 Ertapenem | 11 | 27.3 | 0 | 4.20×10-7 - 1.10×10-5 | ||||
| 美罗培南 Meropenem | 11 | 0 | 0 | ND | ||||
| 多利培南 Doripenem | 11 | 0 | 0 | ND | ||||
| 厄他培南 Ertapenem | 医院分离株 | 140 | 改良PAP | 35 | 2 | ND | 美国 | [ |
| 亚胺培南 Imipenem | 20 | 25 | ||||||
| 美罗培南 Meropenem | 100 | 30 | ||||||
| 亚胺培南 Imipenem | 医院分离株 | 332 | 纸片扩散,E-test(抑菌圈内菌落生长确定为异质性) | 25 | 0 | 8.00×10-8- 1.80×10-7 | 中国重庆 | [ |
| 厄他培南 Ertapenem | 17.2 | 0.6 | ||||||
| 美罗培南 Meropenem | 3.9 | |||||||
| 亚胺培南 Imipenem | 医院分离株 | 200 | E-test(抑菌圈内菌落生长确定为异质性) PAP(异质性耐药以MIC/NIC≥8来确定) | 29 | 0 | ND | 中国广西 | [ |
| 厄他培南 Ertapenem | 20.5 | |||||||
| 美罗培南 Meropenem | 6 | 0.5 | ||||||
| 亚胺培南 Imipenem | 血液、尿液和痰液 | 850 | K-B纸片法 E-test PAP(异质性耐药以MIC/NIC≥8来确定) | 20.5 | 0 | ND | 中国广东 | [ |
| 厄他培南 Ertapenem | 17.5 | 1.5 | ||||||
| 美罗培南 Meropenem | 7 | 0.5 |
表2 大肠埃希菌对碳青霉烯类抗菌药物异质性耐药的流行情况
Table 2 Prevalence of heteroresistance of E. coli to carbapenems
| 抗菌药物 名称 Antibiotic | 样品(来源) Sample (Sources) | 样本数 Number of samples | 异质性耐药测定方法Method for determination of heteroresistance | 异质性耐药率 Prevalence of heteroresistance/% | 耐药率Prevalence of resistance/% | 异质性耐药亚群的频次 Frequency of heteroresistant subpopulations | 国家/地区Country /Region | 文献 Reference |
|---|---|---|---|---|---|---|---|---|
| 亚胺培南 Imipenem | 医院分离株 | 11 | E-test(抑菌圈内菌落生长初步判定异质性) PAP(异质性耐药以MIC/NIC≥8来确定) | 0 | 0 | ND | 瑞典 | [ |
| 厄他培南 Ertapenem | 11 | 27.3 | 0 | 4.20×10-7 - 1.10×10-5 | ||||
| 美罗培南 Meropenem | 11 | 0 | 0 | ND | ||||
| 多利培南 Doripenem | 11 | 0 | 0 | ND | ||||
| 厄他培南 Ertapenem | 医院分离株 | 140 | 改良PAP | 35 | 2 | ND | 美国 | [ |
| 亚胺培南 Imipenem | 20 | 25 | ||||||
| 美罗培南 Meropenem | 100 | 30 | ||||||
| 亚胺培南 Imipenem | 医院分离株 | 332 | 纸片扩散,E-test(抑菌圈内菌落生长确定为异质性) | 25 | 0 | 8.00×10-8- 1.80×10-7 | 中国重庆 | [ |
| 厄他培南 Ertapenem | 17.2 | 0.6 | ||||||
| 美罗培南 Meropenem | 3.9 | |||||||
| 亚胺培南 Imipenem | 医院分离株 | 200 | E-test(抑菌圈内菌落生长确定为异质性) PAP(异质性耐药以MIC/NIC≥8来确定) | 29 | 0 | ND | 中国广西 | [ |
| 厄他培南 Ertapenem | 20.5 | |||||||
| 美罗培南 Meropenem | 6 | 0.5 | ||||||
| 亚胺培南 Imipenem | 血液、尿液和痰液 | 850 | K-B纸片法 E-test PAP(异质性耐药以MIC/NIC≥8来确定) | 20.5 | 0 | ND | 中国广东 | [ |
| 厄他培南 Ertapenem | 17.5 | 1.5 | ||||||
| 美罗培南 Meropenem | 7 | 0.5 |
| 抗菌药物 名称 Antibiotic | 样品(来源) Sample(Sources) | 样本数 Number of samples | 异质性耐药测定方法 Method for determination of heteroresistance | 异质性耐药率 Prevalence of heteroresistance/% | 耐药率 Prevalence of resistance/% | 异质性耐药亚群的频次 Frequency of heteroresistant subpopulations | 国家/地区Country / Region | 文献 Reference |
|---|---|---|---|---|---|---|---|---|
| 黏菌素 Colistin | 临床分离株 | 11 | E-test(抑菌圈内菌落生长初步判定异质性) PAP(异质性耐药以MIC/NIC≥8来确定) | 0 | 0 | ND | 瑞典 | [ |
| 多黏菌素B Polymyxin B | 11 | 0 | 0 | ND | ||||
| 黏菌素 Colistin | 血液分离株 | 292 | 琼脂筛选[菌落生长在黏菌素(4 mg/L)确定为异质性耐药)] | 3.4 | 0.3 | 1.25×10-8-1.10×10-5 | 匈牙利 | [ |
| 黏菌素 Colistin | 医院分离株 | 291 | PAP(异质性耐药以MIC/NIC≥8来确定) PAP | 1.37 | 0.69 | 4.00×10-7-4.00×10-6 | 中国温州 | [ |
| 黏菌素 Colistin | 猪病料样本、猪肛门拭子 | 177 | PAP(异质性耐药以MIC/NIC≥4来确定) | 91.67 | 0 | 6.61×10-7-2.57×10-6 | 中国郑州 | [ |
表3 大肠埃希菌对粘菌素类抗菌药物异质性耐药的流行情况
Table 3 Prevalence of heteroresistance of E. coli to colistin antibiotics
| 抗菌药物 名称 Antibiotic | 样品(来源) Sample(Sources) | 样本数 Number of samples | 异质性耐药测定方法 Method for determination of heteroresistance | 异质性耐药率 Prevalence of heteroresistance/% | 耐药率 Prevalence of resistance/% | 异质性耐药亚群的频次 Frequency of heteroresistant subpopulations | 国家/地区Country / Region | 文献 Reference |
|---|---|---|---|---|---|---|---|---|
| 黏菌素 Colistin | 临床分离株 | 11 | E-test(抑菌圈内菌落生长初步判定异质性) PAP(异质性耐药以MIC/NIC≥8来确定) | 0 | 0 | ND | 瑞典 | [ |
| 多黏菌素B Polymyxin B | 11 | 0 | 0 | ND | ||||
| 黏菌素 Colistin | 血液分离株 | 292 | 琼脂筛选[菌落生长在黏菌素(4 mg/L)确定为异质性耐药)] | 3.4 | 0.3 | 1.25×10-8-1.10×10-5 | 匈牙利 | [ |
| 黏菌素 Colistin | 医院分离株 | 291 | PAP(异质性耐药以MIC/NIC≥8来确定) PAP | 1.37 | 0.69 | 4.00×10-7-4.00×10-6 | 中国温州 | [ |
| 黏菌素 Colistin | 猪病料样本、猪肛门拭子 | 177 | PAP(异质性耐药以MIC/NIC≥4来确定) | 91.67 | 0 | 6.61×10-7-2.57×10-6 | 中国郑州 | [ |

图1 异质性耐药判定标准的推荐方案(改自文献[31]) (1)纸片扩散试验应根据CLSI和BSAC等机构推荐的标准化抗菌药物敏感性试验程序进行。(2)根据CFU计数的PAP应通过在含抗菌药物的琼脂平板上接种10倍连续稀释的细菌培养物来进行。(3)琼脂平板制备应遵循通过琼脂稀释试验测定MIC的标准指南。(4)浊度PAP应遵循肉汤稀释技术测定MIC的标准指南,但每个抗菌药物浓度下细菌生长的浊度定量除外
Fig. 1 Recommended scheme for determination of heteroresistance(Modified from reference[31]) (1)Disc diffusion assays should be performed according to standardized procedures for antimicrobial susceptibility testing as recommended by agencies such as CLSI and BSAC.(2)PAP by CFU counts should be performed by plating aliquots of 10-fold serially diluted bacterial cultures on antibiotic-containing agar plates.(3)Agar plate preparation should follow standardized guidelines for MIC determination by agar dilution assays. Turbidimetric PAP should follow standard guidelines for MIC determination by the broth dilution technique,with the exception of turbidimetric quantification of bacterial growth at each antibiotic concentration
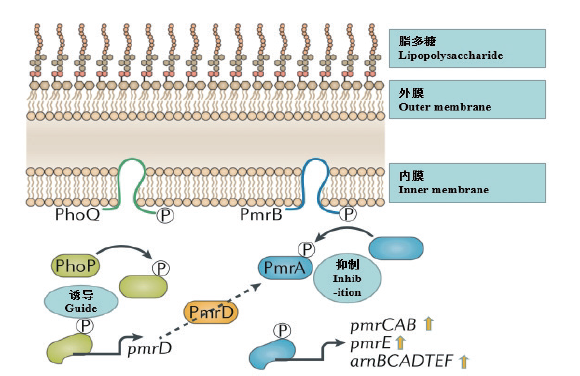
图3 革兰氏阴性菌中PmrAB和PhoPQ双组分系统调节的黏菌素异质性耐药性(改自文献[2])
Fig. 3 Heteroresistance of colistin regulated by PmrAB and PhoPQ in Gram negative bacteria(Modified from reference[2])
| 抗菌药物 Antibiotic | 异质性耐药机制 Heteroresistance mechanism | 参考文献 References |
|---|---|---|
| 头孢菌素类 Cephalosporins | 在携带绿色荧光蛋白基因的质粒上将编码头孢菌素水解酶的blaCTX-M-14基因导入敏感的E.coli菌株,由于与绿色荧光蛋白的融合,在单细胞水平上出现了异质性耐药。 | [ |
| 四环素类 Tetracyclines | 耐药亚群中外排泵相关基因如AcrAB-Tolc、OqxAB、acrAB、oqxAB等表达水平增加或活性增强有关。 | [ |
| 磷霉素 Fosfomycin | 耐药亚群中转运调控基因突变导致磷霉素摄取系统缺陷及磷霉素耐药基因murA过度表达是引起异质性耐药的原因 | [ |
表4 大肠埃希菌对其他抗菌药物的异质性耐药机制
Table 4 Heteroresistance mechanism of E.coli to other antibiotics
| 抗菌药物 Antibiotic | 异质性耐药机制 Heteroresistance mechanism | 参考文献 References |
|---|---|---|
| 头孢菌素类 Cephalosporins | 在携带绿色荧光蛋白基因的质粒上将编码头孢菌素水解酶的blaCTX-M-14基因导入敏感的E.coli菌株,由于与绿色荧光蛋白的融合,在单细胞水平上出现了异质性耐药。 | [ |
| 四环素类 Tetracyclines | 耐药亚群中外排泵相关基因如AcrAB-Tolc、OqxAB、acrAB、oqxAB等表达水平增加或活性增强有关。 | [ |
| 磷霉素 Fosfomycin | 耐药亚群中转运调控基因突变导致磷霉素摄取系统缺陷及磷霉素耐药基因murA过度表达是引起异质性耐药的原因 | [ |
| [1] | 全国细菌耐药监测网, 2020年全国细菌耐药监测报告[EB/OL]. 2020. |
| National Bacterial Resistance Monitoring Network, Henan Agricultural University, 2020 National Bacterial Resistance Monitoring report[EB/OL]. 2020. | |
| [2] |
Andersson DI, Nicoloff H, Hjort K. Mechanisms and clinical relevance of bacterial heteroresistance[J]. Nat Rev Microbiol, 2019, 17(8):479-496.
doi: 10.1038/s41579-019-0218-1 pmid: 31235888 |
| [3] | Charretier Y, Diene SM, Baud D, et al. Colistin heteroresistance and involvement of the PmrAB regulatory system in Acinetobacter baumannii[J]. Antimicrob Agents Chemother, 2018, 62(9):e00788-e00718. |
| [4] |
Altrichter T, Heizmann WR. Gardnerella vaginalis:transport, microscopy, testing resistance[J]. Geburtshilfe Frauenheilkd, 1994, 54(11):606-611.
doi: 10.1055/s-2007-1022350 URL |
| [5] |
Alexander HE, Leidy G. Mode of action of streptomycin on type b Hemophilus influenzae:ii. nature of resistant variants[J]. J Exp Med, 1947, 85(6):607-621.
doi: 10.1084/jem.85.6.607 pmid: 19871639 |
| [6] |
Hiramatsu K, Hanaki H, Ino T, et al. Methicillin-resistant Staphylo-coccus aureus clinical strain with reduced vancomycin susceptibility[J]. J Antimicrob Chemother, 1997, 40(1):135-136.
doi: 10.1093/jac/40.1.135 URL |
| [7] |
El-Halfawy OM, Valvano MA. Antimicrobial heteroresistance:an emerging field in need of clarity[J]. Clin Microbiol Rev, 2015, 28(1):191-207.
doi: 10.1128/CMR.00058-14 pmid: 25567227 |
| [8] |
Li PY, Huang Y, Yu L, et al. Isolation and whole-genome sequence analysis of the imipenem heteroresistant Acinetobacter baumannii clinical isolate HRAB-85[J]. Int J Infect Dis, 2017, 62:94-101.
doi: 10.1016/j.ijid.2017.07.005 URL |
| [9] |
Dewachter L, Fauvart M, Michiels J. Bacterial heterogeneity and antibiotic survival:understanding and combatting persistence and heteroresistance[J]. Mol Cell, 2019, 76(2):255-267.
doi: S1097-2765(19)30733-6 pmid: 31626749 |
| [10] |
Stojowska-Swędrzyńska K, Łupkowska A, Kuczyńska-Wiśnik D, et al. Antibiotic heteroresistance in Klebsiella pneumoniae[J]. Int J Mol Sci, 2021, 23(1):449.
doi: 10.3390/ijms23010449 URL |
| [11] |
Nicoloff H, Hjort K, et al. The high prevalence of antibiotic heteroresistance in pathogenic bacteria is mainly caused by gene amplification[J]. Nat Microbiol, 2019, 4(3):504-514.
doi: 10.1038/s41564-018-0342-0 pmid: 30742072 |
| [12] |
van Hal SJ, Wehrhahn MC, Barbagiannakos T, et al. Performance of various testing methodologies for detection of heteroresistant vancomycin-intermediate Staphylococcus aureus in bloodstream isolates[J]. J Clin Microbiol, 2011, 49(4):1489-1494.
doi: 10.1128/JCM.02302-10 URL |
| [13] | Norazah A, Law NL, Kamel AGM, et al. The presence of heterogeneous vancomycin-lntermediate Staphylococcus aureus(heteroVISA)in a major Malaysian hospital[J]. Med J Malaysia, 2012, 67(3):269-273. |
| [14] |
Lo-Ten-Foe JR, de Smet AMGA, Diederen BMW, et al. Comparative evaluation of the VITEK 2, disk diffusion, etest, broth microdilution, and agar dilution susceptibility testing methods for colistin in clinical isolates, including heteroresistant Enterobacter cloacae and Acinetobacter baumannii strains[J]. Antimicrob Agents Chemother, 2007, 51(10):3726-3730.
pmid: 17646414 |
| [15] |
Leonard SN, Rossi KL, Newton KL, et al. Evaluation of the Etest GRD for the detection of Staphylococcus aureus with reduced susceptibility to glycopeptides[J]. J Antimicrob Chemother, 2009, 63(3):489-492.
doi: 10.1093/jac/dkn520 pmid: 19136530 |
| [16] |
Satola SW, Farley MM, et al. Comparison of detection methods for heteroresistant vancomycin-intermediate Staphylococcus aureus, with the population analysis profile method as the reference method[J]. J Clin Microbiol, 2011, 49(1):177-183.
doi: 10.1128/JCM.01128-10 pmid: 21048008 |
| [17] |
Silveira AC, Sambrano GE, Paim TG, et al. Is prediffusion test an alternative to improve accuracy in screening hVISA strains and to detect susceptibility to glycopeptides/lipopeptides?[J]. Diagn Microbiol Infect Dis, 2014, 79(4):401-404.
doi: 10.1016/j.diagmicrobio.2014.04.008 URL |
| [18] |
Wootton M, Howe RA, Hillman R, et al. A modified population analysis profile(PAP)method to detect hetero-resistance to vancomycin in Staphylococcus aureus in a UK hospital[J]. J Antimicrob Chemother, 2001, 47(4):399-403.
doi: 10.1093/jac/47.4.399 URL |
| [19] | Chakravorty S, Simmons AM, Rowneki M, et al. The new xpert MTB/RIF ultra:improving detection of Mycobacterium tuberculosis and resistance to rifampin in an assay suitable for point-of-care testing[J]. mBio, 2017, 8(4):e00812-e00817. |
| [20] | Sun L, Talarico S, Yao LN, et al. Droplet digital PCR-based detection of clarithromycin resistance in Helicobacter pylori isolates reveals frequent heteroresistance[J]. J Clin Microbiol, 2018, 56(9):e00019-e00018. |
| [21] |
Operario DJ, Koeppel AF, Turner SD, et al. Prevalence and extent of heteroresistance by next generation sequencing of multidrug-resistant tuberculosis[J]. PLoS One, 2017, 12(5):e0176522.
doi: 10.1371/journal.pone.0176522 URL |
| [22] | Tan KR, Nguyen J, Nguyen K, et al. Prevalence of the carbapenem-heteroresistant phenotype among ESBL-producing Escherichia coli and Klebsiella pneumoniae clinical isolates[J]. J Antimicrob Chemother, 2020, 75(6):1506-1512. |
| [23] | Sun JD, Huang SF, Yang SS, et al. Impact of carbapenem heteroresistance among clinical isolates of invasive Escherichia coli in Chongqing, southwestern China[J]. Clin Microbiol Infect, 2015, 21(5):469. e1-469. 10. |
| [24] | 汤丽霞, 韦莹慧, 等. 大肠埃希菌碳青霉烯异质性耐药的流行病学特征及影响因素分析[J]. 右江民族医学院学报, 2018, 40(2):172-176. |
| Tang LX, Wei YH, et al. Epidemiological characteristics and influencing factors analysis of Carbapenems heteroresistant Escherichia coli[J]. J Youjiang Med Univ Natl, 2018, 40(2):172-176. | |
| [25] | 张文萍, 张秋萍, 崔海燕, 等. 大肠埃希菌碳青霉烯异质性耐药分析及流行病学调查[J]. 广东医学, 2018, 39(12):1830-1835. |
| Zhang WP, Zhang QP, Cui HY, et al. Epidemiology and heterogeneous drug resistance of Escherichia coli[J]. Guangdong Med J, 2018, 39(12):1830-1835. | |
| [26] |
Baroud M, Dandache I, et al. Underlying mechanisms of carbapenem resistance in extended-spectrum β-lactamase-producing Klebsiella pneumoniae and Escherichia coli isolates at a tertiary care centre in Lebanon:role of OXA-48 and NDM-1 carbapenemases[J]. Int J Antimicrob Agents, 2013, 41(1):75-79.
doi: 10.1016/j.ijantimicag.2012.08.010 URL |
| [27] |
Zhang CM, Xu XY, Pu SL, et al. Characterization of carbapenemases, extended spectrum β-lactamases, quinolone resistance and aminoglycoside resistance determinants in carbapenem-non-susceptible Escherichia coli from a teaching hospital in Chongqing, Southwest China[J]. Infect Genet Evol, 2014, 27:271-276.
doi: 10.1016/j.meegid.2014.07.031 URL |
| [28] |
Juhász E, Iván M, Pintér E, et al. Colistin resistance among blood culture isolates at a tertiary care centre in Hungary[J]. J Glob Antimicrob Resist, 2017, 11:167-170.
doi: S2213-7165(17)30147-9 pmid: 28838854 |
| [29] |
Liao WL, Lin J, Jia HY, et al. Resistance and heteroresistance to colistin in Escherichia coli isolates from Wenzhou, China[J]. Infect Drug Resist, 2020, 13:3551-3561.
doi: 10.2147/IDR.S273784 URL |
| [30] | 邝启红. 动物源大肠杆菌对黏菌素和头孢噻呋异质性耐药的特性研究[D]. 郑州: 河南农业大学, 2021. |
| Kuang QH. The characteristics of heteroresistance to colistin and ceftiofur in Escherichia coli isolates from animals[D]. Zhengzhou: Henan Agricultural University, 2021. | |
| [31] |
El-Halfawy OM, Valvano MA. Chemical communication of antibiotic resistance by a highly resistant subpopulation of bacterial cells[J]. PLoS One, 2013, 8(7):e68874.
doi: 10.1371/journal.pone.0068874 URL |
| [32] |
Adler M, Anjum M, Andersson DI, et al. Influence of acquired β-lactamases on the evolution of spontaneous carbapenem resistance in Escherichia coli[J]. J Antimicrob Chemother, 2013, 68(1):51-59.
doi: 10.1093/jac/dks368 URL |
| [33] |
Walsh TR, Toleman MA, et al. Metallo-beta-lactamases:the quiet before the storm?[J]. Clin Microbiol Rev, 2005, 18(2):306-325.
doi: 10.1128/CMR.18.2.306-325.2005 URL |
| [34] |
He JC, Jia XJ, Yang SS, et al. Heteroresistance to carbapenems in invasive Pseudomonas aeruginosa infections[J]. Int J Antimicrob Agents, 2018, 51(3):413-421.
doi: 10.1016/j.ijantimicag.2017.10.014 URL |
| [35] | 孙坤玲. 大肠埃希菌碳青霉烯异质性耐药分子机制研究及碳青霉烯酶表型检测方法评价[D]. 重庆: 重庆医科大学, 2017. |
| Sun KL. Molecular mechanism of carbapenem heteroresistance among Escherichia coli and evaluation of six phenotypic methods for the identification of carbapenemases[D]. Chongqing: Chongqing Medical University, 2017. | |
| [36] | 代佳伶. 肺炎克雷伯菌和大肠埃希菌碳青霉烯异质性耐药及机制研究[D]. 重庆: 重庆医科大学, 2019. |
| Dai JL. Study on the mechanism of cabapenem heteroresistance in Klebsiella pneumoniae and Escherichia coli[D]. Chongqing: Chongqing Medical University, 2019. | |
| [37] |
Thulin E, Sundqvist M, Andersson DI. Amdinocillin(Mecillinam)resistance mutations in clinical isolates and laboratory-selected mutants of Escherichia coli[J]. Antimicrob Agents Chemother, 2015, 59(3):1718-1727.
doi: 10.1128/AAC.04819-14 URL |
| [38] | Schechter LM, Creely DP, Garner CD, et al. Extensive gene amplification as a mechanism for piperacillin-tazobactam resistance in Escherichia coli[J]. mBio, 2018, 9(2):e00583-e00518. |
| [39] |
Lee JY, Choi MJ, Choi HJ, et al. Preservation of acquired colistin resistance in gram-negative bacteria[J]. Antimicrob Agents Chemother, 2015, 60(1):609-612.
doi: 10.1128/AAC.01574-15 URL |
| [40] |
Halaby T, Kucukkose E, Janssen AB, et al. Genomic characterization of colistin heteroresistance in Klebsiella pneumoniae during a nosocomial outbreak[J]. Antimicrob Agents Chemother, 2016, 60(11):6837-6843.
doi: 10.1128/AAC.01344-16 URL |
| [41] |
Huang L, Feng Y, Zong ZY. Heterogeneous resistance to colistin in Enterobacter cloacae complex due to a new small transmembrane protein[J]. J Antimicrob Chemother, 2019, 74(9):2551-2558.
doi: 10.1093/jac/dkz236 URL |
| [42] |
Cannatelli A, Giani T, D'Andrea MM, et al. MgrB inactivation is a common mechanism of colistin resistance in KPC-producing Klebsiella pneumoniae of clinical origin[J]. Antimicrob Agents Chemother, 2014, 58(10):5696-5703.
doi: 10.1128/AAC.03110-14 pmid: 25022583 |
| [43] | Kuang QH, He DD, Sun HR, et al. R 93 P substitution in the PmrB HAMP domain contributes to colistin heteroresistance in Escherichia coli isolates from swine[J]. Antimicrob Agents Chemother, 2020, 64(11):e01509-e01520. |
| [44] | Sato T, Shiraishi T, Hiyama Y, et al. Contribution of novel amino acid alterations in PmrA or PmrB to colistin resistance in mcr-negative Escherichia coli clinical isolates, including major multidrug-resistant lineages O25b:H4-ST131-H 30Rx and Non-x[J]. Antimicrob Agents Chemother, 2018, 62(9):e00864-e00818. |
| [45] |
Liu YY, Wang Y, Walsh TR, et al. Emergence of plasmid-mediated colistin resistance mechanism MCR-1 in animals and human beings in China:a microbiological and molecular biological study[J]. Lancet Infect Dis, 2016, 16(2):161-168.
doi: 10.1016/S1473-3099(15)00424-7 URL |
| [46] | Xavier BB, Lammens C, et al. Identification of a novel plasmid-mediated colistin-resistance gene, mcr-2, in Escherichia coli, Belgium, June 2016[J]. Euro Surveill, 2016, 21(27):30280. |
| [47] | Yin WJ, Li H, Shen YB, et al. Novel plasmid-mediated colistin resistance gene mcr-3 in Escherichia coli[J]. mBio, 2017, 8(3):e00543-e00517. |
| [48] |
Lippa AM, Goulian M. Feedback inhibition in the PhoQ/PhoP signaling system by a membrane peptide[J]. PLoS Genet, 2009, 5(12):e1000788.
doi: 10.1371/journal.pgen.1000788 URL |
| [49] | Rodríguez-Villodres Á, Ortiz de la Rosa JM, Álvarez-Marín R, et al. Heteroresistance to piperacillin-tazobactam in clinical isolates of Escherichia coli sequence type 131[J]. Antimicrob Agents Chemother, 2017, 62(1):e01923-e01917. |
| [50] |
Cohen SP, McMurry LM, Levy SB. marA locus causes decreased expression of OmpF porin in multiple-antibiotic-resistant(Mar)mutants of Escherichia coli[J]. J Bacteriol, 1988, 170(12):5416-5422.
pmid: 2848006 |
| [51] | 刘宇阳, 蓝锴, 等. 耐碳青霉烯类大肠埃希菌对替加环素异质性耐药的机制[J]. 分子诊断与治疗杂志, 2021, 13(2):178-182. |
| Liu YY, Lan K, et al. Mechanisms of tigecycline heteroresistance in carbapenem-resistant Escherichia coli[J]. J Mol Diagn Ther, 2021, 13(2):178-182. | |
| [52] | Lucas AE, Ito R, Mustapha MM, et al. Frequency and mechanisms of spontaneous fosfomycin nonsusceptibility observed upon disk diffusion testing of Escherichia coli[J]. J Clin Microbiol, 2017, 56(1):e01368-e01317. |
| [53] |
Campos A, Andrade NL, Couto N, et al. Characterization of fosfomycin heteroresistance among multidrug-resistant Escherichia coli isolates from hospitalized patients in Rio de Janeiro, Brazil[J]. J Glob Antimicrob Resist, 2020, 22:584-593.
doi: 10.1016/j.jgar.2020.04.026 URL |
| [54] | Wang XR, Kang Y, Luo CX, et al. Heteroresistance at the single-cell level:adapting to antibiotic stress through a population-based strategy and growth-controlled interphenotypic coordination[J]. mBio, 2014, 5(1):e00942-e00913. |
| [55] |
Lebeaux D, Ghigo JM, Beloin C. Biofilm-related infections:bridging the gap between clinical management and fundamental aspects of recalcitrance toward antibiotics[J]. Microbiol Mol Biol Rev, 2014, 78(3):510-543.
doi: 10.1128/MMBR.00013-14 URL |
| [56] |
Bisht K, Wakeman CA. Discovery and therapeutic targeting of differentiated biofilm subpopulations[J]. Front Microbiol, 2019, 10:1908.
doi: 10.3389/fmicb.2019.01908 pmid: 31507548 |
| [57] |
Naparstek L, Carmeli Y, Navon-Venezia S, et al. Biofilm formation and susceptibility to gentamicin and colistin of extremely drug-resistant KPC-producing Klebsiella pneumoniae[J]. J Antimicrob Chemother, 2014, 69(4):1027-1034.
doi: 10.1093/jac/dkt487 pmid: 24408988 |
| [58] | Serra DO, Richter AM, Klauck G, et al. Microanatomy at cellular resolution and spatial order of physiological differentiation in a bacterial biofilm[J]. mBio, 2013, 4(2):e00103-e00113. |
| [59] |
Silva A, Sousa AM, et al. Heteroresistance to colistin in Klebsiella pneumoniae is triggered by small colony variants sub-populations within biofilms[J]. Pathog Dis, 2016, 74(5):ftw036.
doi: 10.1093/femspd/ftw036 URL |
| [1] | 江润海, 姜冉冉, 朱城强, 侯秀丽. 微生物强化植物修复铅污染土壤的机制研究进展[J]. 生物技术通报, 2023, 39(8): 114-125. |
| [2] | 王天依, 王荣焕, 王夏青, 张如养, 徐瑞斌, 焦炎炎, 孙轩, 王继东, 宋伟, 赵久然. 玉米矮秆基因与矮秆育种研究[J]. 生物技术通报, 2023, 39(8): 43-51. |
| [3] | 张蓓, 任福森, 赵洋, 郭志伟, 孙强, 刘贺娟, 甄俊琦, 王童童, 程相杰. 辣椒响应热胁迫机制的研究进展[J]. 生物技术通报, 2023, 39(7): 37-47. |
| [4] | 李典典, 粟元, 李洁, 许文涛, 朱龙佼. 抗菌适配体的筛选与应用进展[J]. 生物技术通报, 2023, 39(6): 126-132. |
| [5] | 张和臣, 袁欣, 高杰, 王校晨, 王慧娟, 李艳敏, 王利民, 符真珠, 李保印. 植物花瓣呈色机理及花色分子育种[J]. 生物技术通报, 2023, 39(5): 23-31. |
| [6] | 易希, 廖红东, 郑井元. 植物内生真菌防治根结线虫研究进展[J]. 生物技术通报, 2023, 39(3): 43-51. |
| [7] | 王伟宸, 赵进, 黄薇颐, 郭芯竹, 李婉颖, 张卓. 芽胞杆菌代谢产物防治三种常见植物病原真菌的研究进展[J]. 生物技术通报, 2023, 39(3): 59-68. |
| [8] | 崔吉洁, 蔡文波, 庄庆辉, 高爱平, 黄建峰, 陈亚辉, 宋志忠. 杧果Fe-S簇装配基因MiISU1的生物学功能[J]. 生物技术通报, 2023, 39(2): 139-146. |
| [9] | 李凯航, 王浩臣, 程可心, 杨艳, 金一, 何晓青. 全基因组关联分析研究植物与微生物组的互作遗传机制[J]. 生物技术通报, 2023, 39(2): 24-34. |
| [10] | 罗宁, 焦阳, 茆振川, 李惠霞, 谢丙炎. 木霉菌对根结线虫和孢囊线虫防治机理研究进展[J]. 生物技术通报, 2023, 39(2): 35-50. |
| [11] | 陈广霞, 李秀杰, 蒋锡龙, 单雷, 张志昌, 李勃. 植物小分子信号肽参与非生物逆境胁迫应答的研究进展[J]. 生物技术通报, 2023, 39(11): 61-73. |
| [12] | 王晨宇, 周楚源, 何堤, 樊梓豪, 王梦梦, 杨柳燕. 多聚磷酸盐在微生物抗环境胁迫中的作用及机制[J]. 生物技术通报, 2023, 39(11): 168-181. |
| [13] | 齐方婷, 黄河. 观赏植物花斑形成调控机制的研究进展[J]. 生物技术通报, 2023, 39(10): 17-28. |
| [14] | 刘佳欣, 张会龙, 邹荣松, 杨秀艳, 朱建峰, 张华新. 不同类型盐生植物适应盐胁迫的生理生长机制及Na+逆向转运研究进展[J]. 生物技术通报, 2023, 39(1): 59-72. |
| [15] | 金云倩, 王彬, 郭书磊, 赵霖熙, 韩赞平. 赤霉素调控玉米种子活力的研究进展[J]. 生物技术通报, 2023, 39(1): 84-94. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||